Understanding Atrial Fibrillation: A Comprehensive Guide
Atrial fibrillation is a common heart condition that requires understanding and management to prevent complications.
What is Atrial Fibrillation?
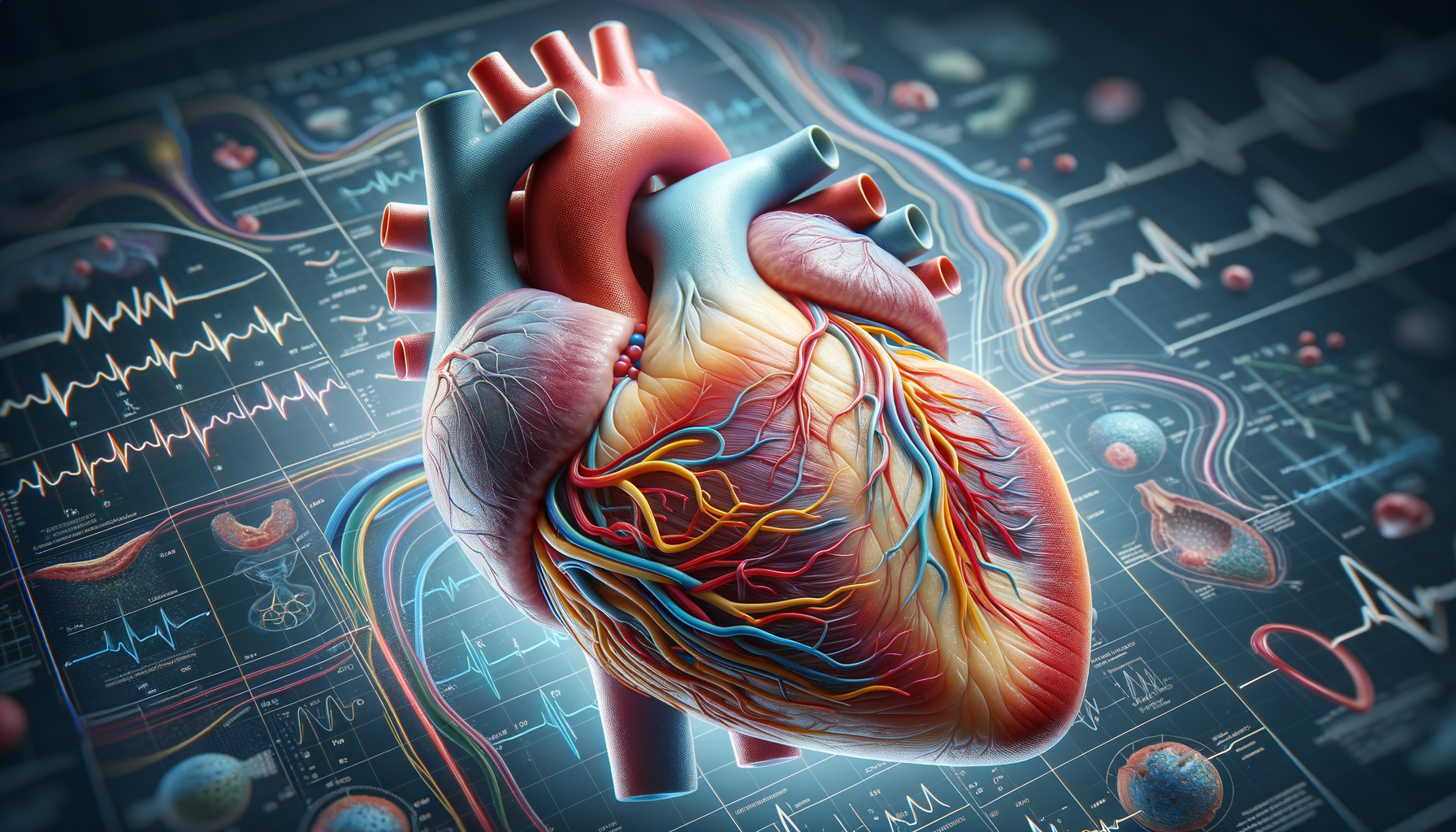
Atrial fibrillation, often abbreviated as AFib, is a type of irregular heartbeat that can lead to blood clots, stroke, heart failure, and other heart-related complications. It occurs when the upper chambers of the heart (the atria) beat irregularly and out of coordination with the lower chambers (the ventricles). This can result in a rapid and chaotic heart rhythm, which may cause symptoms like heart palpitations, shortness of breath, and fatigue.
AFib is significant because it is the most common type of arrhythmia, affecting millions of people globally. The prevalence of atrial fibrillation increases with age, and it is more common in individuals with other heart conditions or risk factors such as hypertension, diabetes, and obesity. Understanding AFib is crucial for managing its effects and reducing the risk of complications.
Causes and Risk Factors
The causes of atrial fibrillation are varied and can include both lifestyle factors and pre-existing health conditions. Some common causes are:
- High blood pressure, which can strain the heart and lead to AFib.
- Heart diseases such as coronary artery disease and heart valve disorders.
- Excessive alcohol consumption, which can affect heart rhythm.
- Thyroid problems, particularly hyperthyroidism.
Risk factors for developing AFib include age, family history, and lifestyle choices. For instance, individuals over the age of 60 are at a higher risk, as are those with a family history of the condition. Additionally, unhealthy lifestyle choices such as smoking, prolonged stress, and lack of physical activity can increase the likelihood of developing AFib.
Symptoms and Diagnosis
Symptoms of atrial fibrillation can vary greatly among individuals. Some people may experience noticeable symptoms, while others may have none at all. Common symptoms include:
- Heart palpitations or fluttering sensations in the chest.
- Shortness of breath, especially during physical activity.
- Fatigue and weakness.
- Dizziness or lightheadedness.
Diagnosing AFib typically involves a physical examination and the use of diagnostic tools such as an electrocardiogram (ECG), which records the electrical activity of the heart. In some cases, a Holter monitor or event recorder may be used to capture heart activity over a longer period.
Management and Treatment Options
Treating atrial fibrillation involves a combination of lifestyle changes, medication, and sometimes surgical interventions. The primary goals of treatment are to restore a normal heart rhythm, prevent blood clots, and manage risk factors. Common treatment options include:
- Medications such as beta-blockers, calcium channel blockers, and anticoagulants.
- Lifestyle changes like reducing alcohol intake, quitting smoking, and maintaining a healthy weight.
- Procedures like electrical cardioversion, which uses electrical shocks to restore a normal heart rhythm.
In some cases, surgical options such as catheter ablation or the implantation of a pacemaker may be recommended to manage AFib more effectively.
Living with Atrial Fibrillation
Living with atrial fibrillation requires ongoing management and lifestyle adjustments to reduce the risk of complications. Regular medical check-ups are essential to monitor the condition and adjust treatment plans as needed. Patients are often advised to:
- Follow a heart-healthy diet rich in fruits, vegetables, and whole grains.
- Engage in regular physical activity, as recommended by a healthcare provider.
- Manage stress through techniques such as meditation, yoga, or deep-breathing exercises.
Support groups and educational resources can also be beneficial for individuals with AFib, providing a sense of community and additional information on managing the condition effectively.