Understanding Ulcerative Colitis: Symptoms and Treatments
Introduction to Ulcerative Colitis
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Characterized by inflammation and ulceration of the innermost lining of the large intestine, this condition can lead to a variety of symptoms that significantly impact a person’s quality of life. Understanding the symptoms and treatments of ulcerative colitis is crucial for managing the disease effectively and improving patient outcomes.
Ulcerative colitis is part of a group of diseases known as inflammatory bowel diseases, which also includes Crohn’s disease. These conditions are often confused due to their similar symptoms, but they affect different parts of the gastrointestinal tract and have distinct pathologies. While the exact cause of ulcerative colitis remains unknown, it is believed to result from an abnormal immune response in genetically predisposed individuals. Environmental factors, such as diet and stress, may also play a role in triggering flare-ups.
Recognizing the Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis can vary widely among individuals, ranging from mild to severe. Common symptoms include abdominal pain, cramping, and diarrhea, often accompanied by blood or pus in the stool. Patients may also experience an urgent need to defecate, fatigue, and weight loss. In severe cases, ulcerative colitis can lead to complications such as dehydration, anemia, and increased risk of colon cancer.
Symptoms are often episodic, with periods of remission followed by flare-ups. During remission, symptoms may subside entirely, allowing individuals to lead relatively normal lives. However, during flare-ups, symptoms can become debilitating, necessitating medical intervention. Recognizing the symptoms early and seeking timely medical advice is essential for effective management of the disease.
Beyond the physical symptoms, ulcerative colitis can also have a profound impact on mental health. The unpredictability of flare-ups and the chronic nature of the disease can lead to anxiety and depression. It’s important for patients to seek support from healthcare professionals, support groups, and mental health counselors to address these challenges.
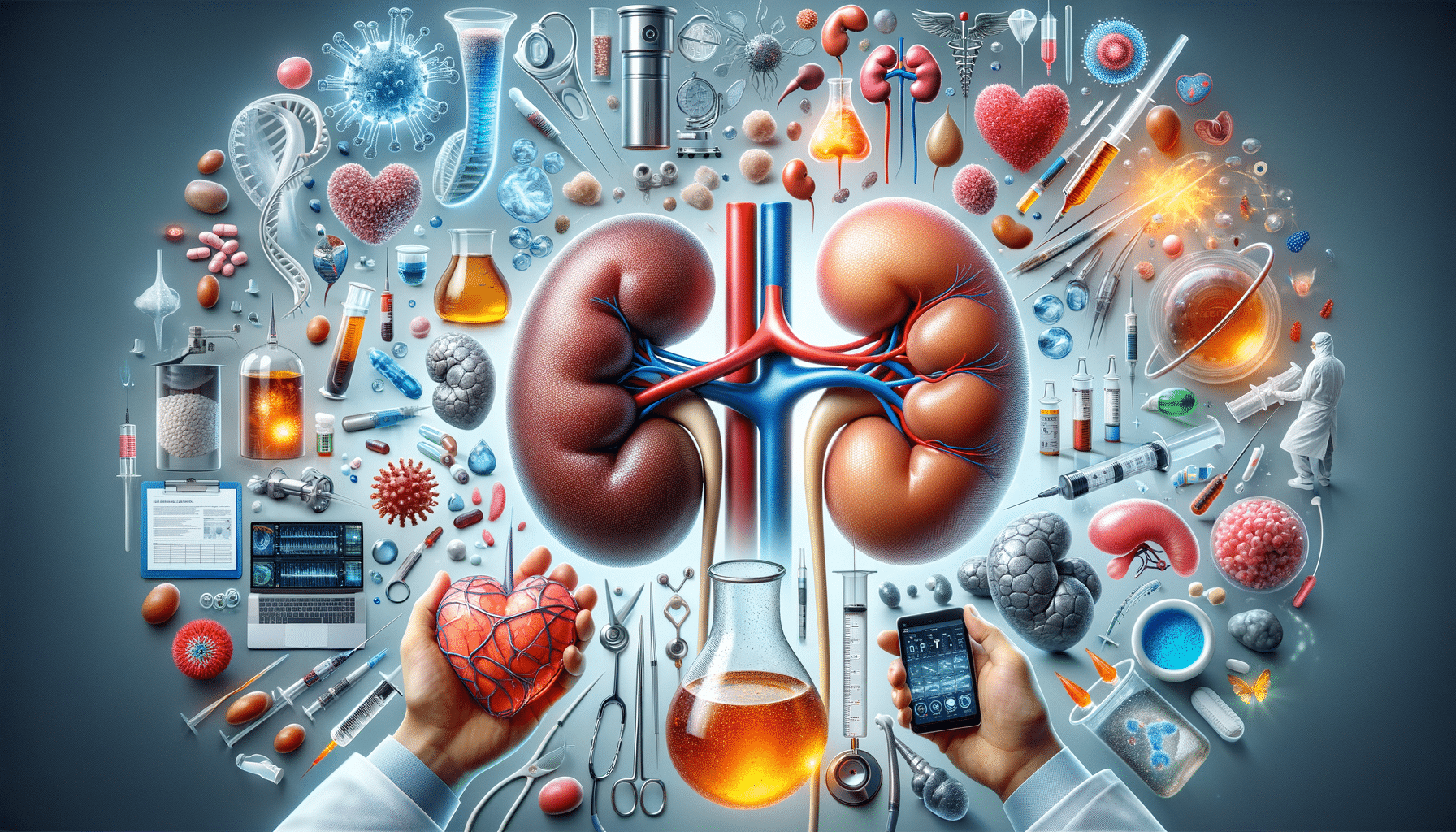
Diagnosing Ulcerative Colitis
Diagnosing ulcerative colitis involves a combination of clinical evaluation, laboratory tests, and imaging studies. Healthcare providers typically begin with a thorough medical history and physical examination, focusing on gastrointestinal symptoms and family history of IBD. Blood tests may be conducted to check for anemia and markers of inflammation, while stool samples can help rule out infections.
Endoscopic procedures, such as colonoscopy and sigmoidoscopy, are crucial for diagnosing ulcerative colitis. These procedures allow direct visualization of the colon and rectum, enabling doctors to assess the extent and severity of inflammation. Biopsies taken during endoscopy can confirm the diagnosis by revealing characteristic histological features of ulcerative colitis.
Imaging studies, such as abdominal X-rays, CT scans, and MRI, may also be used to evaluate complications and rule out other conditions. A comprehensive diagnostic approach ensures accurate diagnosis and helps guide treatment decisions, tailored to the individual needs of each patient.
Treatment Options for Ulcerative Colitis
Treatment for ulcerative colitis aims to reduce inflammation, manage symptoms, and achieve and maintain remission. The choice of treatment depends on the severity of the disease and the patient’s overall health. Medications are the cornerstone of ulcerative colitis treatment and include:
- Aminosalicylates: These anti-inflammatory drugs are often the first line of treatment for mild to moderate ulcerative colitis.
- Corticosteroids: Used for short-term relief during flare-ups, corticosteroids help reduce inflammation quickly.
- Immunomodulators: These medications suppress the immune system to prevent ongoing inflammation.
- Biologics: Targeted therapies that block specific proteins involved in the inflammatory process.
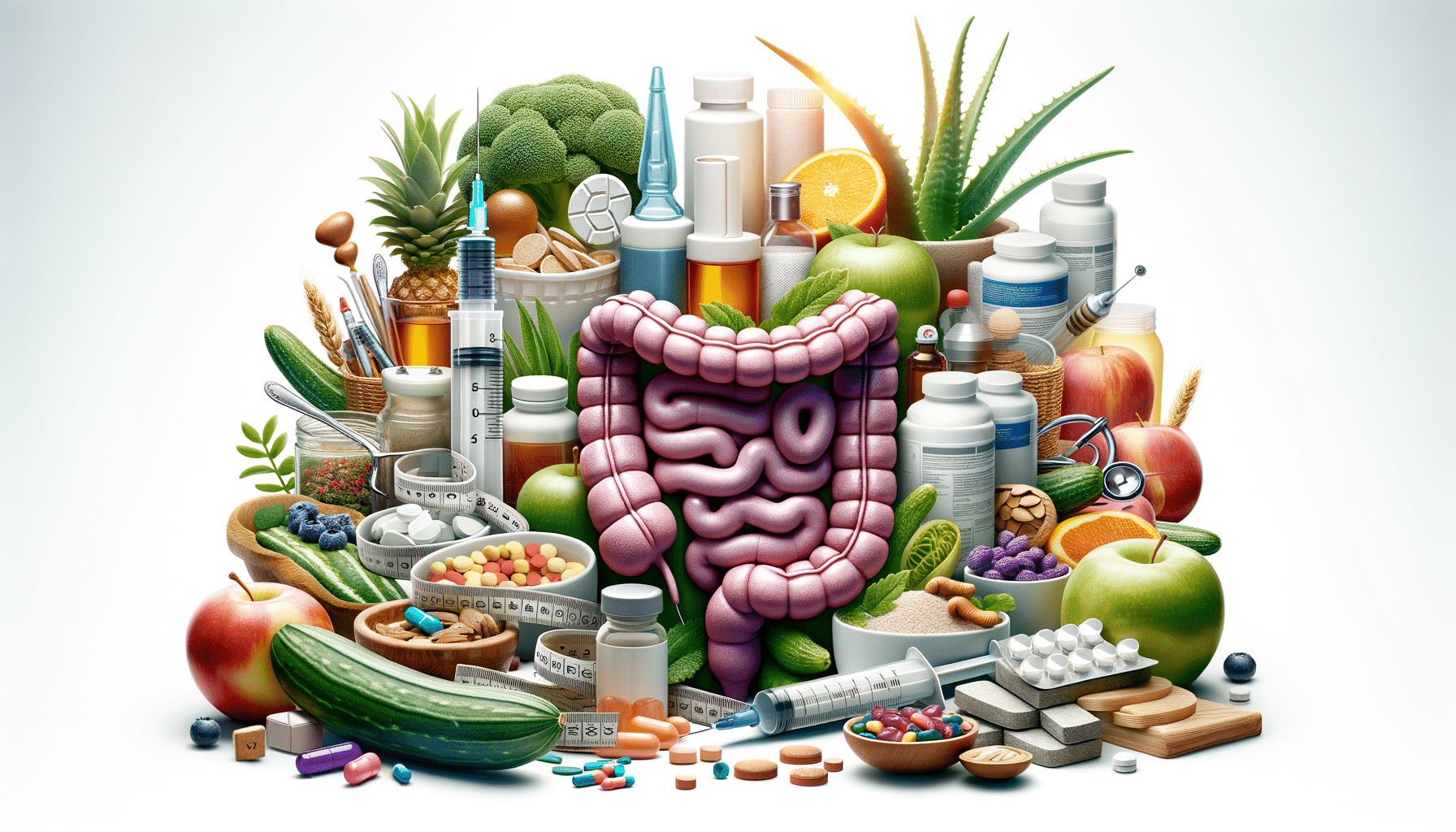
In addition to medication, lifestyle modifications play a crucial role in managing ulcerative colitis. Dietary changes, stress management, and regular exercise can help control symptoms and improve overall well-being. In severe cases, surgery may be necessary to remove the affected portion of the colon, providing a potential cure for ulcerative colitis.
It’s important for patients to work closely with their healthcare team to develop a personalized treatment plan that addresses their unique needs and preferences. Regular follow-up appointments and monitoring are essential to assess treatment efficacy and make necessary adjustments.
Living with Ulcerative Colitis
Living with ulcerative colitis can be challenging, but with the right strategies and support, individuals can lead fulfilling lives. Education and awareness are key to managing the disease effectively. Patients should stay informed about their condition, treatment options, and lifestyle modifications that can help reduce symptoms.
Support from family, friends, and healthcare providers is invaluable. Joining support groups and connecting with others who have ulcerative colitis can provide emotional support and practical advice. Mental health care should not be overlooked, as managing stress and anxiety is crucial for overall well-being.
Adopting a proactive approach to health can empower individuals with ulcerative colitis to take control of their condition. Regular medical check-ups, adherence to treatment plans, and open communication with healthcare providers are essential components of effective disease management. By staying informed and engaged, individuals with ulcerative colitis can navigate the challenges of their condition and enjoy a good quality of life.