Treatment Strategies for Ulcerative Colitis Flare-Ups
Understanding Ulcerative Colitis Flare-Ups
Ulcerative colitis is a chronic inflammatory bowel disease that primarily affects the colon and rectum. It is characterized by periods of remission and flare-ups, where symptoms like abdominal pain, diarrhea, and rectal bleeding become more pronounced. Understanding the nature of these flare-ups is crucial for effective management and treatment.
Flare-ups can be triggered by various factors, including stress, dietary choices, infections, or even changes in medication. These episodes can significantly impact a person’s quality of life, making it essential to have a comprehensive understanding of the condition. During a flare-up, the immune system mistakenly attacks the lining of the colon, leading to inflammation and ulceration.
While the exact cause of ulcerative colitis remains unknown, genetic, environmental, and immune system factors are believed to play a role. Recognizing the symptoms early and seeking prompt medical attention can help in managing the condition effectively. It’s a collaborative effort between patients and healthcare providers to identify triggers and develop personalized treatment plans.
Medical Treatments for Ulcerative Colitis Flare-Ups
Medical treatment is often the first line of defense against ulcerative colitis flare-ups. The goal is to reduce inflammation, manage symptoms, and maintain remission. Various medications are available, and the choice depends on the severity of the flare-up and the patient’s response to previous treatments.
Common medications include:
- Aminosalicylates: These are often used to treat mild to moderate flare-ups and help maintain remission.
- Corticosteroids: These are used for short-term relief during moderate to severe flare-ups due to their powerful anti-inflammatory effects.
- Immunomodulators: These help reduce immune system activity and are often used for long-term management.
- Biologics: These are newer treatments that target specific components of the immune system and are used for moderate to severe cases.
It’s essential to work closely with a healthcare provider to determine the most appropriate medication regimen. Regular monitoring and adjustments may be necessary to ensure optimal management of the condition.
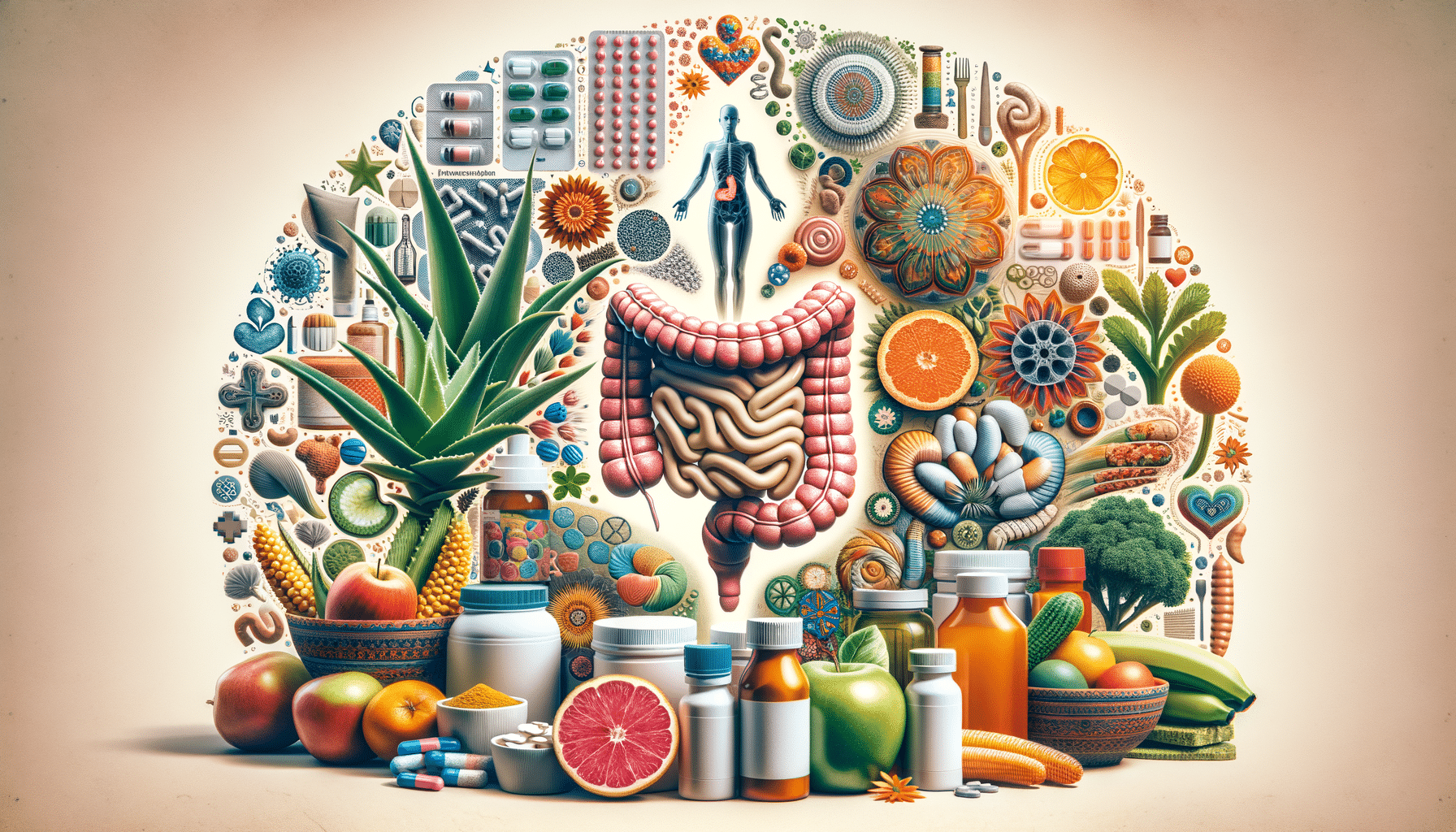
Diet and Lifestyle Modifications
In addition to medication, diet and lifestyle play a significant role in managing ulcerative colitis flare-ups. While there is no one-size-fits-all diet for everyone with ulcerative colitis, certain dietary adjustments can help alleviate symptoms and prevent flare-ups.
Some general dietary recommendations include:
- Identifying and avoiding trigger foods that worsen symptoms.
- Maintaining a balanced diet rich in nutrients to support overall health.
- Staying hydrated to prevent dehydration from diarrhea.
- Considering smaller, more frequent meals to ease digestion.
Lifestyle changes, such as stress management techniques, regular exercise, and adequate sleep, can also contribute to better management of the condition. Stress is a known trigger for flare-ups, so incorporating relaxation techniques like yoga or meditation can be beneficial.
Alternative and Complementary Therapies
For some individuals, alternative and complementary therapies may offer additional relief during ulcerative colitis flare-ups. While these should not replace conventional medical treatments, they can be used in conjunction to enhance overall well-being.
Popular complementary therapies include:
- Probiotics: These beneficial bacteria may help restore balance in the gut microbiome.
- Herbal supplements: Some herbs, like turmeric, have anti-inflammatory properties that may aid in symptom management.
- Acupuncture: This traditional Chinese medicine technique may help reduce stress and improve digestive health.
It’s essential to discuss any alternative therapies with a healthcare provider to ensure they are safe and appropriate for individual circumstances. Personal experiences with these therapies can vary, so it’s important to monitor their effects closely.
Long-Term Management and Prevention
Managing ulcerative colitis is a lifelong journey that requires ongoing attention and care. Preventing flare-ups and maintaining remission are key objectives for individuals living with this condition. Long-term management involves a combination of medical treatment, lifestyle adjustments, and regular monitoring.
Key strategies for long-term management include:
- Adhering to prescribed medication regimens even during remission to prevent flare-ups.
- Regular check-ups with healthcare providers to monitor disease progression and adjust treatments as needed.
- Staying informed about new research and treatment options that may improve quality of life.
- Building a support network of healthcare professionals, family, and support groups to provide guidance and encouragement.
By taking a proactive approach, individuals with ulcerative colitis can lead fulfilling lives and minimize the impact of flare-ups on their daily activities.